
Cavities are holes in the teeth that form from tooth decay. Although prevalence varies across Australian states and territories, the Australian Institute of Health and Welfare estimates that 42% of children between the ages of 5 and 10 have cavities in their baby teeth. Even though many people associate cavities as a childhood health obstacle, it’s a more prevalent problem in adults. Tooth decay affects over 90% of the Australian adult population.
Because of the widespread prevalence, you may be wondering, “How can I tell if I have a cavity? How do dentists treat cavities?” Below, we answer these questions and more.
What are the common symptoms of cavities?
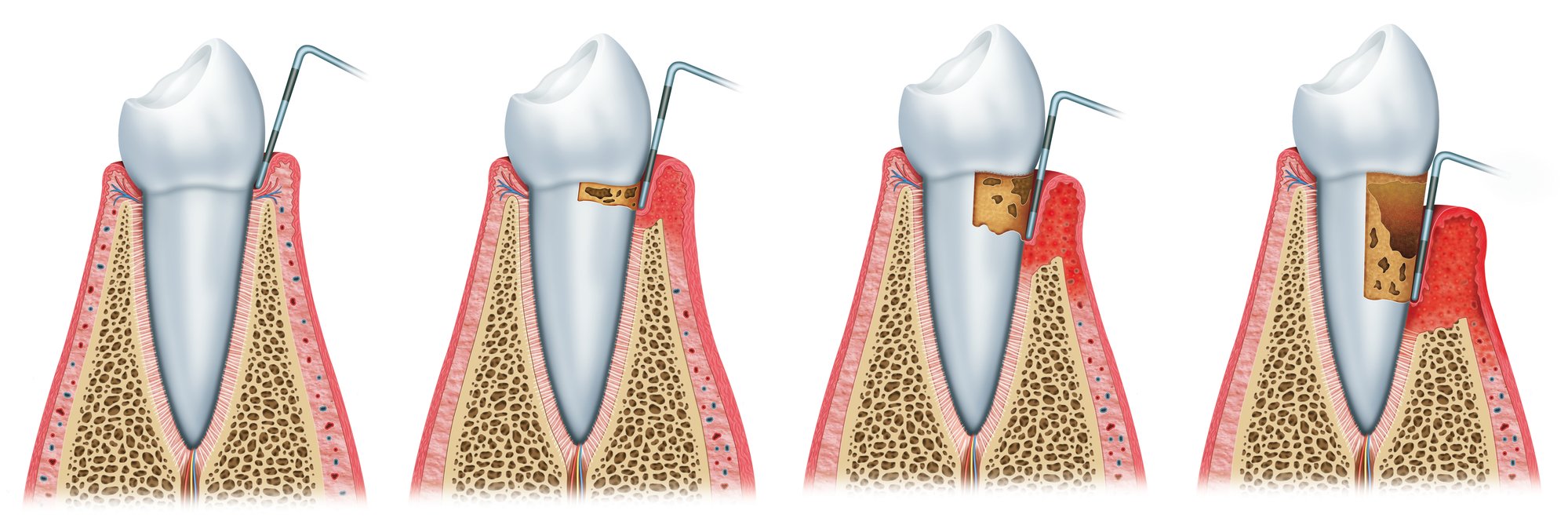
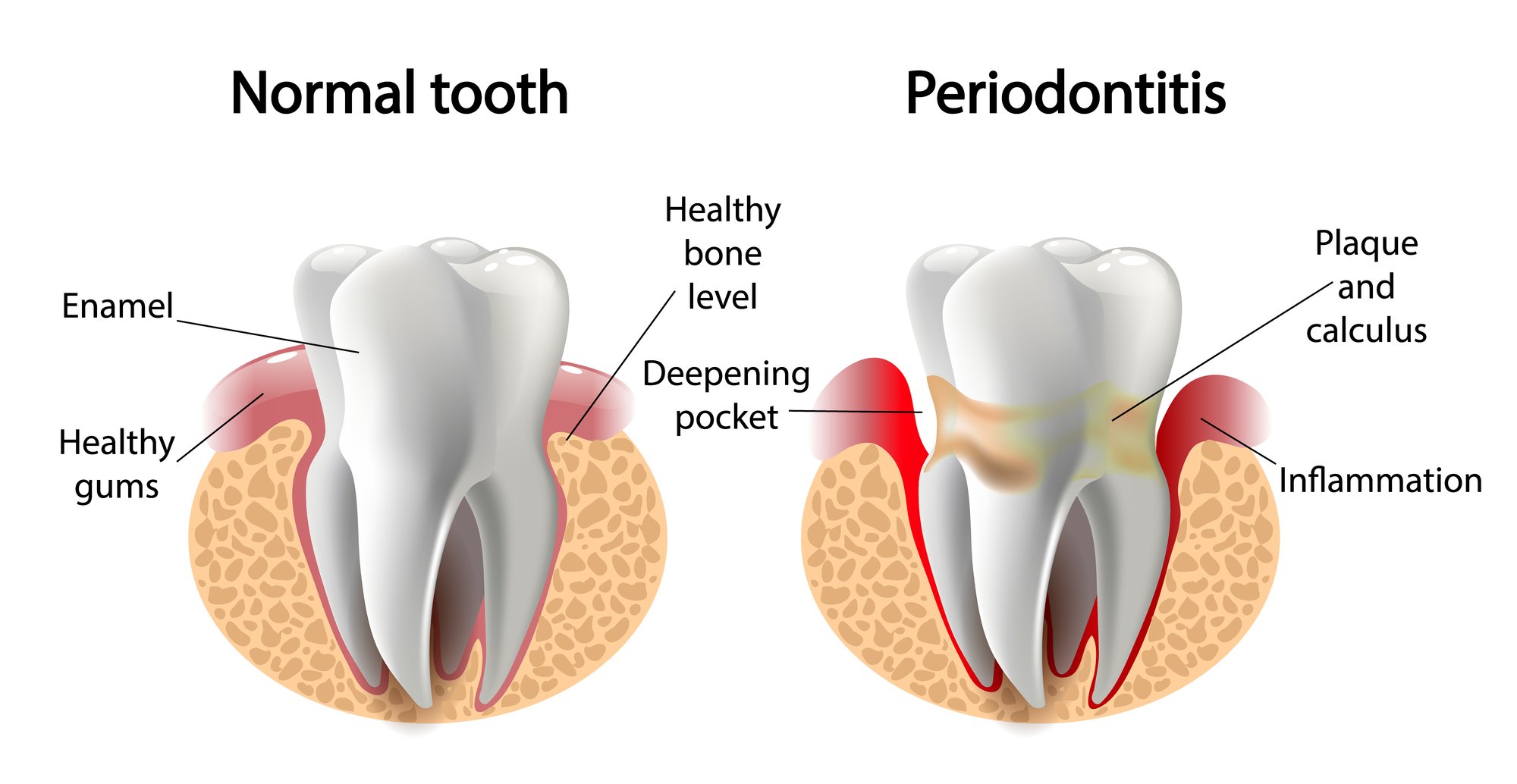
Plaque (a sticky film of bacteria) constantly forms on the teeth. When people eat or drink foods with sugar or carbohydrates, they feed the oral bacteria in plaque. Consequently, the bacteria excrete acids that destroy the tooth enamel (the hard surface of the teeth). If not removed, the enamel breaks down and forms holes in the teeth (cavities).
If you believe that you or your loved one may have tooth decay, below are three common cavity symptoms to keep an eye out for:
1. Discomfort
Even though cavities do not usually cause pain until they are deep enough to affect the underlying nerves and tissues, a toothache is one of the most apparent symptoms. Discomfort can fluctuate from mild to intolerable. Also, toothaches can come abruptly, continuously, or promptly when biting, chewing, or eating.
2. Sensitivity
Below the enamel, the dentin has two roles (1) to reinforce the tooth’s enamel and (2) to protect the pulp chamber that houses the blood vessels and nerves deep inside the tooth. As the enamel erodes, the dentin is more exposed, and the dental nerves are more stimulated. As a result, sensitivity may occur after consuming food and drinks that are too hot, cold, acidic, sweet, or sticky.
3. Enamel Changes
As cavity-causing bacteria chemically changes the tooth, there may be changes of appearance:
- Staining: White, brown, or black spots are the beginning visual signs of tooth decay. As the spots worsen, they become darker (brown or black) and more extensive.
- Holes and pits: As staining advances, it can change into a hole or pit in the tooth. They may be noticeable by sight or felt when the tongue is run over the surface of the teeth. Sometimes, they may be difficult to see or feel if they are in ridges on the molars (the back of the mouth) or between the teeth.
How do dentists treat cavities?
While cavities may start small and unnoticeable, they rapidly expand when left untreated. After a dentist removes the decayed tissues, they may restore the tooth with a dental filling or crown.
If you are experiencing cavities symptoms, contact us now.
Many people are unaware of when a cavity forms. However, a dentist can identify tooth decay before it causes alarming symptoms that lead to more severe challenges with regular check-ups. At Magic Smiles Dental, Dr. Arpit Pathak offers a wide range of treatments to prevent and heal tooth decay for patients of all ages.
If you or your loved one are experiencing any of the listed cavity symptoms, we advise that you seek care immediately. The sooner that you seek care, the greater your odds are at preventing tooth decay progression. To schedule an appointment, contact us online or call one of our many New South Wales locations:
- Woolgoolga: (02) 6654-0650
- Coffs Harbour: (02) 6652-3242








Recent Comments